We know there are a lot of burning questions out there.
What happens when we die?
What is the secret of the Bermuda Triangle?
Who killed JFK?
Are we alone in the universe?
Surely, up there with all your burning questions, you are brimming with curiosity about Haglund’s Syndrome. While we may never know exactly what happened to Amelia Earhart or the Mayan Empire, we do know a thing or two about Haglund’s Syndrome. Here are the top questions about Haglund’s Syndrome and their answers.
Q: What is Haglund’s Syndrome?
A: Haglund’s Syndrome, also known as Haglund’s Deformity, is a bony bump on the back of a heel. It is typically painful.
Q: What are the symptoms of Haglund’s Syndrome?
A: A few defining symptoms of Haglund’s Syndrome include:
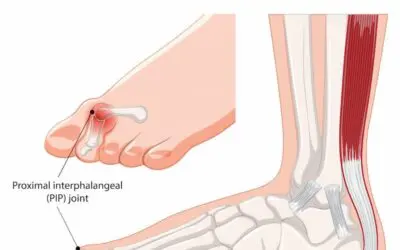
- A bony bump at the back of the heel near the Achilles tendon
- Swollen bursa sac, which manifests itself as swollen tissue near the bony protrusion
- Severe heel pain at the bony bump
- Redness and inflammation around the bump
- Callus around the inflamed area
Q: How did I get Haglund’s Syndrome?
A: Haglund’s Syndrome is caused by constant pressure on the back of the heel. This can be caused by heels that are too stiff in the back or shoes that are too tight.
Q: Is Haglund’s Syndrome the same as a “pump bump?”
A: Yes. Haglund’s Syndrome developed the nickname “pump bump” because women who regularly wear stiff high-heeled pumps often develop bony protrusion.
Q: What risk factors increase my chance of developing Haglund’s Syndrome?
A: A couple of different risk factors may contribute to the development of Haglund’s Syndrome:
- A tendency to walk on the outside of your heel
- High arches
- Tight Achilles tendons
- Running on hard surfaces
- Running uphill
- Genetics
Q: What is bursitis, and what does it have to do with Haglund’s Syndrome?
A: Bursitis is when the bursa sac is inflamed. Bursa sacs exist in all your joints, and they help cushion all the bones, muscles, and tendons. Bursitis can accompany Haglund’s Syndrome if the condition irritates the bursa sac near the Achilles tendon.
Q: How can I alleviate pain caused by Haglund’s Syndrome?
A: Treating the symptoms will help ease the pain in your heel. Some ideas may include the following:
- Ice the painful area
- Changing your footwear to something that does not rub against the back of your foot or something that is soft
- Wear custom orthotics
- Perform exercises that strengthen the Achilles tendon, such as heel lifts
- Receive ultrasound treatments from a podiatrist or physical therapist
- Take over-the-counter anti-inflammatory pain medication such as Ibuprofen or acetaminophen
- Give yourself soft tissue massages
- Do some physical therapy
- Invest in heel pads
- Receive steroid injections
- Wear an immobilizing boot
- Have surgery
Q: Is surgery inevitable for everyone who has Haglund’s Syndrome?
A: You may be able to reduce your symptoms significantly through the non-invasive treatments above. These conservative measures should be used first, and they may be successful on their own. If they are unsuccessful, then you can discuss surgery options, including calcaneoplasty, with your foot and ankle specialist.
Q: What is an endoscopic calcaneoplasty?
A: This mouthful is the surgery that removes the bony protrusion from Haglund’s Syndrome. It is performed by creating two small incisions, and then a camera and special instruments then allow the surgeon to cut down the bone (and possibly do some reconstruction work on the Achilles tendon while they are in there).
Q: What is recovery from endoscopic calcaneoplasty like?
A: Plan on wearing a surgical boot for up to a month after an endoscopic calcaneoplasty. Once the boot is off, you can begin building up the strength in your Achilles area again. If you heal well, you might be able to return to regular activity three months after the surgery.
Q: Who can I talk to about potential Haglund’s Syndrome?
A: If you suspect you have Haglund’s Syndrome developing on your heel, a podiatrist will be able to help you.
Q: Should I see a podiatrist about my suspected Haglund’s Syndrome, or should I wait to see if it heals on its own?
A: Don’t delay seeking care for your painful bump. Regardless of the diagnosis, the sooner you can receive professional help, the sooner you can be pain-free and healthy.
For answers to any questions about Haglund’s Syndrome we missed, contact a local podiatry office today.