You’re gliding through the water, each stroke a gentle rhythm that feels as easy as breathing. Swimming seems like the perfect escape—a low-impact sport that offers a full-body workout—until you step out of the pool, that is.
From fungal infections and plantar warts to foot cramps and overuse injuries, swimming can lead to a variety of foot issues. If left untreated, these injuries can impact your ability to move comfortably—both in and out of the pool.
But don’t worry—with a bit of know-how, some preventive care, and the help of a foot pain specialist, you can keep your feet as strong and healthy as your strokes.
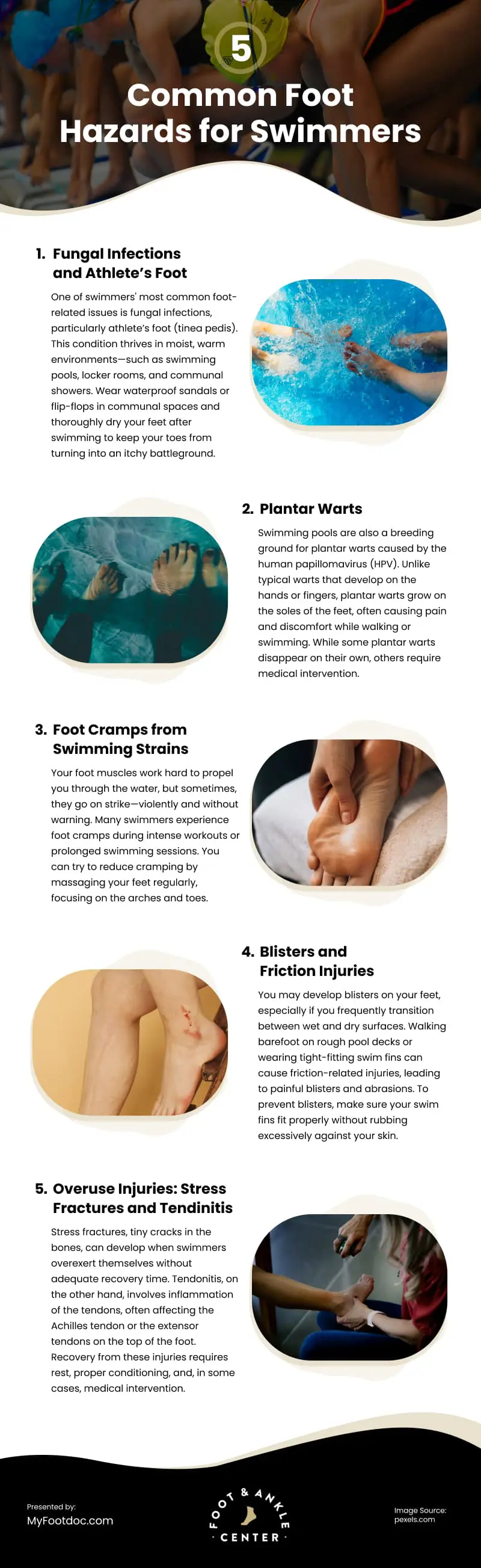
Common Foot Hazards for Swimmers
1. Fungal Infections and Athlete’s Foot
One of swimmers’ most common foot-related issues is fungal infections, particularly athlete’s foot (tinea pedis).
This condition thrives in moist, warm environments—such as swimming pools, locker rooms, and communal showers. The fungus responsible for athlete’s foot can linger on wet surfaces, quickly spreading through direct contact with contaminated floors or shared footwear. Where there’s moisture, there’s mischief.
If you have a bad case of the itchies and scratchies, you may have athlete’s foot. Other symptoms include burning sensations, peeling skin, and blisters, often beginning between the toes. If not treated promptly, the infection can spread to different areas of the foot, giving you discomfort and an increased risk of secondary bacterial infections—when it rains, it pours.
Wear waterproof sandals or flip-flops in communal spaces and thoroughly dry your feet after swimming to keep your toes from turning into an itchy battleground. Use antifungal powders or sprays if needed. If your case is persistent, talk to a podiatrist about athlete’s foot treatments. They may recommend prescription-strength medications to eliminate the infection and prevent recurrence.
2. Plantar Warts
Swimming pools are also a breeding ground for plantar warts caused by the human papillomavirus (HPV). Unlike typical warts that develop on the hands or fingers, plantar warts grow on the soles of the feet, often causing pain and discomfort while walking or swimming.
Plantar warts are highly contagious and can be contracted by walking barefoot on contaminated pool decks, locker room floors, or showers. They appear as small, rough, callus-like growths, sometimes with tiny black dots in the center. The pressure from walking or swimming can force these warts deeper into the skin, making them more painful.
While some plantar warts disappear on their own, others require medical intervention. Search for a “podiatrist with plantar wart removal near me” to learn about various treatment options, such as cryotherapy (freezing the wart), laser treatments, or surgical removal in severe cases.
Plantar warts are like tiny, unwelcome stowaways—you might not notice them hitching a ride, but once they’re on board, they’re a real pain.
3. Foot Cramps from Swimming Strains
Your foot muscles work hard to propel you through the water, but sometimes, they go on strike—violently and without warning.
Many swimmers experience foot cramps during intense workouts or prolonged swimming sessions. These sudden, involuntary muscle contractions can happen because of dehydration, electrolyte imbalances, or overuse of the foot muscles while kicking.
Unlike on land, where you can stop and stretch, dealing with a cramp in deep water can be dangerous. A sudden foot cramp can disrupt your stroke, leading to discomfort and potential panic. If you frequently experience foot cramps, it’s time to take preventative measures. Stay well-hydrated, maintain proper potassium and magnesium levels, and stretch before and after swimming.
You can try to reduce cramping by massaging your feet regularly, focusing on the arches and toes. If your cramps persist despite all you can do, consult a specialist who may help identify underlying causes, such as nerve compression or circulation issues.
4. Blisters and Friction Injuries
You may develop blisters on your feet, especially if you frequently transition between wet and dry surfaces. Walking barefoot on rough pool decks or wearing tight-fitting swim fins can cause friction-related injuries, leading to painful blisters and abrasions.
To prevent blisters, make sure your swim fins fit properly without rubbing excessively against your skin. Use moisturizing creams to keep the skin supple and reduce the risk of friction injuries.
Swimming might be low-impact, but your feet won’t get the memo if you’re constantly fighting against rough surfaces, tight gear, or the dreaded pool deck walk.
5. Overuse Injuries: Stress Fractures and Tendinitis
Swimming might feel effortless, but your feet know the truth—too much kicking, pushing, and flipping can leave them overworked and begging for a break.
Stress fractures, tiny cracks in the bones, can develop when swimmers overexert themselves without adequate recovery time. Symptoms include localized pain, swelling, and tenderness along the top or sides of the foot.
Tendonitis, on the other hand, involves inflammation of the tendons, often affecting the Achilles tendon or the extensor tendons on the top of the foot. Prolonged repetitive motions—such as flutter kicks or repeatedly pushing off the pool wall—can lead to chronic pain and stiffness.
Recovery from these injuries requires rest, proper conditioning, and, in some cases, medical intervention. Listen to your body and give your feet the rest they deserve. They’ll keep you gliding through the water, not limping out of it.
When to See a Foot Pain Specialist
You can manage many foot-related swimming injuries with at-home care, but sometimes, seeking professional treatment is necessary. Contact a podiatrist immediately if you experience persistent pain, signs of infection, swelling, or difficulty walking.
Severe cases, such as non-healing stress fractures, advanced plantar warts, or tendon damage, may require surgical intervention. Foot surgeons can perform specialized procedures to restore function and relieve chronic pain.
Ignoring foot pain won’t earn you a gold medal—it can lead to long-term complications, affecting not just swimming performance but also everyday mobility. Early intervention and proper care can prevent minor issues from escalating into serious conditions that require extensive medical treatment.
Conclusion
Swimming is a fantastic sport for overall fitness and rehabilitation, but don’t let foot troubles sink your fun. From fungus and warts to cramps and strains, swimmers face plenty of foot woes.
Stay ahead by wearing protective footwear, practicing proper hygiene, stretching regularly, and listening to your body’s signals. That way, you can enjoy your time in the water without unnecessary pain or injury.
If pain persists, always talk to a podiatrist. After all, happy feet make for a smoother swim.
FAQs
1. Can swimming cause foot pain?
2. How can I prevent athlete’s foot after swimming?
3. Are plantar warts contagious in swimming pools?
4. Why do my feet cramp while swimming?
5. Can swim fins cause foot injuries?
6. What should I do if I develop blisters from swimming?
7. Are stress fractures common in swimmers?
8. How can I protect my feet from infections in public pools?
9. What treatments are available for persistent foot pain after swimming?
10. When should I see a doctor for a swimming-related foot injury?
Infographic
Swimming can lead to several foot problems, including fungal infections, plantar warts, cramps, and overuse injuries. Left untreated, these issues may affect your comfort both in and out of the pool. Check out this infographic to learn about common foot hazards and practical tips for prevention.