Plantar Fasciitis Treatment
You’d think a good night’s rest would help your feet relax and ease the pain. With plantar fasciitis, however, pain is actually worse as you get out of bed and take those first few steps. Pain can make you dread mornings and color your mood. The pain can stop you from taking a morning walk with the dog or going to the gym, making you less active throughout the day. It makes it harder to get out of the car or stand after you’ve been sitting a while, and it can feel like you’re walking on rocks.
So, what is plantar fasciitis? What causes it? Where do you find plantar fasciitis treatment in Mesquite, Nevada, or St. George, Utah?
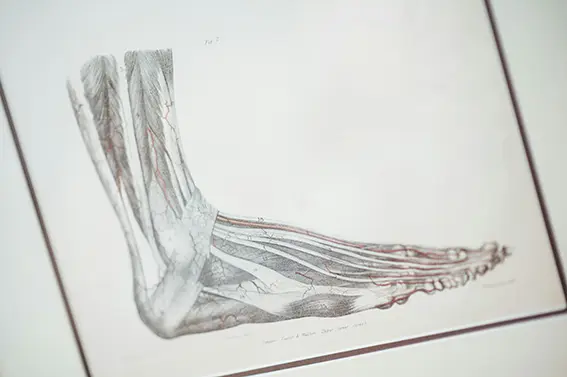
Foot Anatomy
In the foot, you have 26 bones attached to one another by ligaments. Tendons attach muscles and nerves to the bone. They contract and relax in order to make the foot point and flex. Under all of that is a fibrous, thick material that attaches to the heel and runs along the bottom of the foot to the base of the toes. This material is called the plantar fascia, and the tension between the heel and ball of the foot along the fascia helps support your foot arch. The arch absorbs impact and conserves energy by acting like a spring in your feet as you walk, run, or jump. Under the fascia are fat pads designed to cushion your bones when they hit the ground.

Plantar Fasciitis
When you look at a young child, they can squat till their hind ends touch their calves without ever lifting their heel off the ground. Wearing shoes with elevated heels have robbed most adults of the flexibility and balance to do that. And it isn’t just high heels that are the problem, though they have led to a higher number of women with plantar fasciitis than men. Tennis shoes, sandals, and boots all have an elevated heel to limit impact when the heel strikes the ground and to give shoes longevity.
Wearing elevated heels for long periods can cause the fascia to tighten and shrink, a process that is more pronounced at night when you aren’t constantly stretching and flexing your foot. Then, when you step out of bed in the morning, the tightened fascia is forced to stretch, causing pain in the heel and along the bottom of the foot. Sustained tension on the fascia can lead to small tears and inflammation, which increase the pain. Prolonged stress from the plantar fascia pulling on the heel can also cause bone spurs to grow on the heel, so it feels like you’re stepping on a rock.
- Age: Most people develop symptoms between the ages of 40 and 60.
- Extreme Activity: Ballet dancers, long-distance runners, and others who strain their feet are more prone to fasciitis.
- Foot Movement: High arches, fallen arches, abnormal walking patterns, and weight distribution lead to fasciitis. Additionally, fasciitis may cause you to compensate by walking unnaturally to ease the pain, which strains the ankles, knees, hips, and back.
- Being Overweight. Excess weight causes your feet to flatten and pull on the fascia, causing the ankles, knees, and hips to work unnaturally.
- Occupation: People who work all day on their feet, like nurses, or stand on hard floors for long time periods, like factory workers, put unusual strain on the fascia.
Plantar fasciitis is a common malady, but not all treatments are the same. Because there are many contributing factors, each patient is unique, and you deserve a plantar fasciitis doctor who will tailor your treatment to your needs.
R.I.C.E.
If you’re new to plantar fasciitis and are looking for relief, you can start with R.I.C.E.:
Rest: Especially for those who run long distances or dance, giving your feet a break could go a long way toward easing your discomfort. If you can, give them a few days of tender loving care to reduce inflammation. Avoid heels if possible. If not, choose low-heeled shoes with a wider, more stable heel and better support.
Ice: You can put your feet in an ice bath for no longer than 10 minutes. You could also add a little gentle stretching by wearing socks and rolling a frozen water bottle under your foot, concentrating on the arch, or placing ice packs around your feet. Always keep a cloth between you and the ice and limit exposure to 10-15 minutes to avoid skin damage from the cold.
Compression: Give your feet support, especially when doing activities that might cause more inflammation. You can use compression socks or a bandage around the arch and heel. You should be able to stick three fingers between the bandage and your skin to maintain adequate circulation. If your foot starts to throb, loosen the compression bandage.
Elevation: Put your feet up higher than the level of your heart and relax. Inflammation can cause swelling in your feet. This encourages blood to return to your upper body.


Home Remedies
Bed Stretch: Sometimes, a gentle stretch can get you through temporary cases of plantar fasciitis. You can try a stretch before getting out of bed by holding your heel with one hand and using the other hand to gently push your toes up and back. Hold for 10 seconds, relax, and repeat several times. By doing this before you get out of bed, you can limit the pain in those first few steps.
Wall Stretch: Another option is to stretch against a wall. Put your heel on the ground close enough to the wall that the ball of your foot and toes rest on the wall, then lean forward, stretching your calf and plantar fascia.
Rolling Stretch: You can also roll a ball or frozen water bottle under your foot to massage and stretch the fascia.
Tissue Trick: Sometimes plantar fasciitis is caused or exacerbated because it’s compensating for weaker surrounding muscles. A way to strengthen the little muscles in your feet is to pick up a tissue from the ground with your toes. Over time, the muscles will support the foot’s structure better.
Medicine: Over-the-counter anti-inflammatories like Advil (Ibuprofen) or Aleve (Naproxen) will help relieve symptoms.
Shoes: While your feet heal, it can help to wear orthotic shoes with well-cushioned soles to relieve the impact pressure on the heel and midfoot.
Plantar Fasciitis Treatment in Mesquite, Nevada, and St. George, UT
There are a number of different techniques you can pursue to get relief from your plantar fasciitis. However, people with moderate to severe fasciitis may not find enough relief without seeking a plantar fasciitis specialist. Here’s a closer look at some of the treatments you can expect from leading plantar fasciitis podiatrists in Mesquite or St. George:
- Physical Therapy: A specialist can give you specific exercises to strengthen the lower leg muscles so they better support the foot structure when you walk. Tight calves and weak foot muscles can put too much strain on the plantar fascia. The doctor can give you other stretches to loosen the fascia when it gets tight and teach you how to use athletic tape.
- Orthotics: Your podiatrist can recommend specific inserts or custom orthotics to better support your foot. You need the right balance of space and support to lessen the strain on your feet, and sometimes, it’s hard to find that balance going to a regular shoe store.
- Night Splints: Since the fascia tends to tighten overnight in a relaxed position, splints keep your feet immobilized in a position that lengthens the Achilles tendons and the fascia. You’ll have less pain in the morning.
- Adaptive Equipment: As a temporary measure, your podiatrist may recommend a walking boot, walker, crutches, or cane. You’ll put less weight on your foot with assistance.
- Steroid Injection: By injecting a steroid into the inflamed tissue, it can calm the inflammation and ease pain temporarily while you work on other therapies for lasting relief.
- Platelet-Rich Plasma Injection: In your blood, you have plasma (liquid), red cells (transport nutrients and oxygen throughout the body), white cells (protect the body from disease and infection), and platelets (sticky cells that form barriers and stop your body from bleeding). When the medical team separates your blood in a centrifuge, they take plasma and platelets out and cycle the rest of the blood back into your body. The platelets contain growth hormones that encourage rapid healing in several bodily systems. Platelet-rich plasma has been used to help with sports injuries, especially injuries that typically take a long time to heal, like tendons and ligaments. They inject the platelet-rich plasma at the site of a tear in the fascia or some other site of injury to encourage healing.
- Sound Wave Therapy: For those with chronic pain, your podiatrist may recommend something called extracorporeal shock wave plantar fasciitis treatment. Basically, they direct sound waves at the bottoms of your feet to stimulate healing.
- Ultrasonic Repair: Your podiatrist could try repairing torn or damaged tissue when other less invasive options are exhausted. Using ultrasound technology to guide them, they insert a needle-like probe that vibrates to break up damaged tissue before suctioning it out.
- Endoscopic Repair: Utilizing a tiny device with a camera, the surgeon cleans up ragged tissue and removes any bone spurs caused by plantar fasciitis.
- Plantar Fasciitis Surgery: When all other interventions have failed, your surgeon can strategically cut the fascia to release the pressure.
When to Contact a Podiatrist
If plantar fasciitis interferes with your daily activities, alters the way you walk, and doesn’t go away in a few days, you want to consult a podiatrist. There are other conditions that present as plantar fasciitis, and you want to verify what you’re treating, or the treatment may not help. Some of the conditions that mimic plantar fasciitis are:
- Ruptured Fascia: If you’ve had plantar fasciitis for a while or you have impact trauma to the bottom of the foot, the fascia can tear in multiple places all at once. A popping sound often accompanies a ruptured fascia, and you won’t be able to put weight on your foot without experiencing extreme pain.
- Arthritis: Arthritis is chronic inflammation that can degrade bone and cartilage. Like plantar fasciitis, it’s more painful when you step on it first thing in the morning before it has time to loosen up. It also gets more painful with overuse and less painful when you relax. An X-ray can show which condition you’re working with, as arthritis will show wear and tear on bones and joints.
- Peripheral Neuropathy: People who have diabetes, have circulation issues, take certain meds, or are born with certain congenital conditions may experience nerve deterioration. You may feel tingling, buzzing, burning, or stabbing pain.
- Stress Fracture: People who run often or long distances, dance, stand all day on hard surfaces, or experience trauma can develop tiny stress fractures in the heel. Pain will increase with use rather than dissipate. An X-ray will show any cracks in the bone.
- Tibial Nerve Entrapment: Much like carpal tunnel syndrome, there is a bundle of nerves, ligaments, and muscles that squeeze through the tarsal tunnel. The tibial nerve mimics plantar fasciitis when it gets pinched, causing a stabbing or burning sensation in the heel. You might also experience numbness on the bottom of the foot. If you can cause symptoms by moving your foot around while elevated rather than pressed against the floor, it’s not plantar fasciitis.
- Atrophy: The fat pad in your heel protects your bones from impact trauma when you walk, run, dance, or jump. As you age, the fat layer thins, and the bones get painful.
- Bursitis: Just like in your shoulder, wrist, knee, or elbow, there are bursae in your foot. These tiny, fluid-filled sacs cushion bones so they don’t rub against each other. When they get inflamed, they can be painful to the touch. A massage will hurt bursae but will ease the pain of plantar fasciitis.
- Tendonitis: The Achilles tendon can get inflamed or even rupture, causing extreme pain in the heel. The best indicator that it is the tendon and not the plantar fascia is the location of the pain. The tendon attaches at the back of the heel, and the plantar fascia attaches at the front.
Why Plantar Fasciitis Treatment in Mesquite, Nevada and St. George, UT
Dr. Cameron has been a podiatrist and podiatric surgeon since 2016. He opened his own practice, the Foot & Ankle Center, in 2021 in Mesquite, Nevada, and was in such demand that he opened a second office in St. George, Utah, in 2023.
He’s a member of the American Podiatric Medical Association (A.P.M.A.) and the American College of Foot and Ankle Surgeons (A.C.F.A.S.). He has surgical privileges at Mesa View Regional Hospital, St. George Regional Hospital, and Cedar City Hospital.
Dr. Cameron is the one you want working with your child after a sports injury to get them back on the court or in the field. He’ll keep your dancers on the stage and runners on the track. He’s there when you need him and will work with you to protect your family’s long-term health and mobility. If you or a loved one have foot pain, Dr. Cameron offers comprehensive plantar fasciitis treatment. He takes a conservative approach to podiatry, saving surgery as a last resort. However, if surgery is the best option, Dr. Cameron has the experience you need. Call our office today.

